Tiny wireless device might help in combating obesity
Gastric bypass surgery is sometimes the last resort for those who struggle with obesity or serious weight-related health issues. Since this procedure involves making a small stomach pouch and rerouting the digestive tract, it is invasive and prolongs the recovery period for patients.
In a U.S. National Science Foundation-supported study, researchers at Texas A&M University have developed a medical device that might help with weight loss while requiring a simpler operative procedure for implantation.
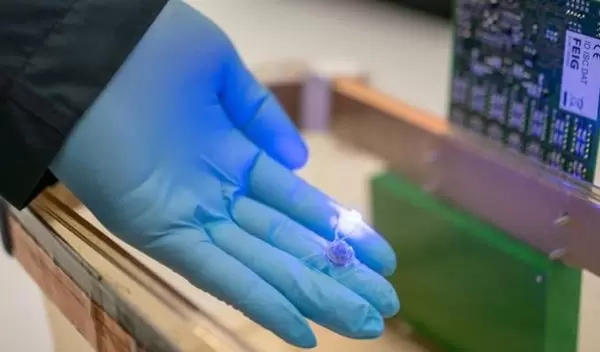
The scientists said their centimeter-sized device provides the feeling of fullness by stimulating the endings of the vagus nerve with light. Unlike other devices that require a power cord, their device is wireless and can be controlled externally from a remote radio frequency source.
"We wanted to create a device that not only requires minimal surgery for implantation but also allows us to stimulate specific nerve endings in the stomach," said Sung II Park, an electrical and computer engineer. "Our device has the potential to do both these things in harsh gastric conditions, which, in the future, can be hugely beneficial to people needing weight loss surgeries."
Further details about the device are published in Nature Communications.
In recent years, the vagus nerve has received attention as a target for treating obesity since it sends sensory information about fullness from the stomach lining to the brain. Although there are medical devices that can stimulate vagus nerve endings and consequently help in curbing hunger, these devices are similar in design to a pacemaker, with wires connected to a current source providing electrical jolts to activate the tips of the nerve.
However, Park said that wireless technology, as well as the application of advanced genetic and optical tools, have the potential to make nerve stimulation devices less cumbersome and more comfortable for the patient.
"These findings could facilitate behavior changes in diabetic patients," says Deborah Jackson, a program director in NSF's Directorate for Engineering.


